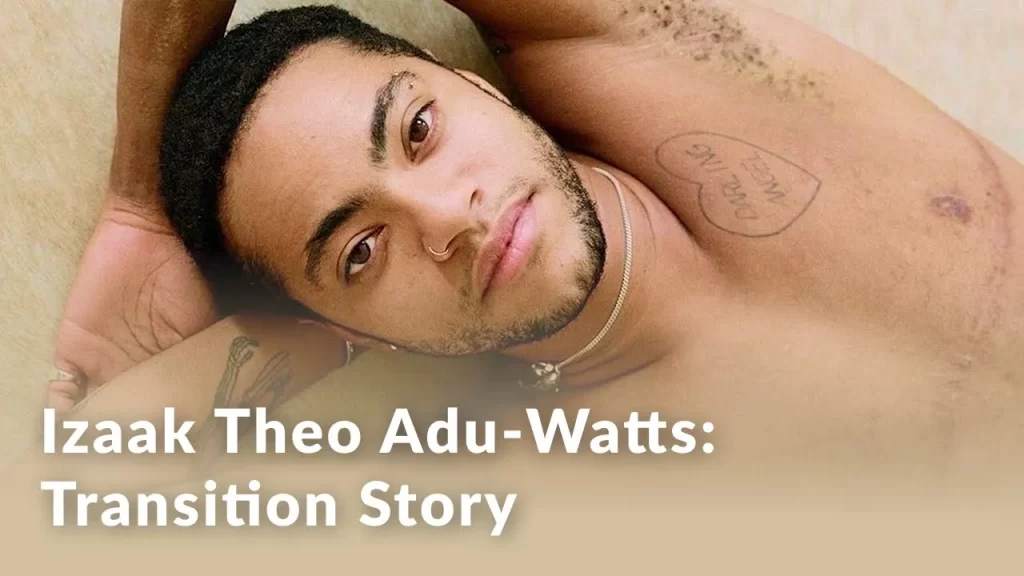
Gender Confirmation Surgery (formerly known as Sexual Reassignment Surgery) entails the surgical process that has enabled thousands of transgender men to complete their transition. This series of surgeries will alter the chest and genitalia to ensure that your gender identity perfectly aligns with your body.
Dr. Christopher Salgado and his team of multidisciplinary experts have come to the aid of many transgender men who were assigned female at birth. Together, these procedures can ease the distress you feel from dysphoria (Gender Identity Disorder) and allow you to become your true self.
How long is gender confirmation surgery?
The whole process takes over one year to complete and depends largely on your goals and the recovery time between procedures.
| PROCEDURE | SURGICAL TIME | RECOVERY |
|---|---|---|
| Chest Masculinization | 1-3 hours Out-patient unless medical problems | First visit at 10 days if admitted to hospital and drains removed at this time; 6 weeks of no strenuous exercise |
| Genitalia | The staged procedure with first stage 3 hours and second stage 8-12 hours | Following the first stage, 3-5 days in hospital then splint removed at 10 days. Following the second stage approximately 2-3 weeks in the hospital |
Female to Male (F2M) Gender Confirmation Surgeries
Gender Confirmation Surgery oversees a number of procedures that will sculpt the chest and genitalia to align your body with your gender identity.
FTM Surgical Procedures
Face
Enhance your facial features and achieve a more masculine appearance through our specialized FMS procedures, tailored to meet the unique needs and goals of individuals undergoing a female to male transition.
Chest
Achieve a more masculine chest contour with our comprehensive procedures, including chest masculinization surgery or breast reduction techniques, helping you achieve a more affirming and masculine chest appearance.
FTM Genitalia
Experience a complete gender affirmation journey with our advanced surgical techniques, allowing for the creation of male genitalia that aligns with your true self and enhances your overall well-being.
Frequently Asked Questions
Mental Health Evaluations from a qualified therapist are required you can begin Hormone Replacement Therapy and Gender Confirmation Surgery. This has been met with understandable resistance from many in the transgender community. While efforts have been made to improve this process, it is important to remember that this safeguards your emotional stability and future since we do adhere to the World Professional Association of Transgender Health Clinical Guidelines.
Also known as Gender Identity Disorder, this describes the emotional conflict transgender people experience.
This enables the change of secondary sexual characteristics to better match your gender identity. It can also do wonders to reduce the emotional stress brought on by gender dysphoria.
No. It is important to keep in mind that all transgender people are unique. The decision to undergo surgery all depends on the level of dysphoria a transgender person experiences in his or her daily life. It all depends on the needs and desires of the individual.
While it is possible to undergo multiple procedures at certain stages of the surgical process, it is not advisable. The body needs time to recover in between surgeries.
Schedule a Consultation
Take the first step towards your transformation. Schedule a consultation with our experienced surgeons today.
Call Us: +786-627-4601